What is Filamentary Keratitis ? |
Filamentary keratitis is a chronic disorder in which filaments, which are adherent complexes of mucus and corneal epithelium, are present on the corneal surface. Filaments consist of a variable combination of degenerated epithelial cells and mucous which are attached to the corneal surface at one end. Filaments present as small, gelatinous strands on the anterior surface of the cornea and may vary in size, shape, composition, and distribution.
Leber in 1882, first described the characteristic threads adherent to anterior surface of the cornea (Leber. Klin Monatsbl f Augenh; 1882. P. 165). Beetham in 1935, published an extensive review and potential therapy options. He outlined that the formation of filaments is due to lacrimal gland destruction and is produced by various systemic reasons viz. infection, lymphoma or hormone dysfunction (Beetham W. Filamentary Keratitis. Trans Am Ophthalmol Soc. 1935; 33: 413-435).
A lack of tear production may result in the increased production of mucous by conjunctival goblet cells. Aqueous-deficient eye is characterised by excessive abnormal debris and mucous strands, which adhere firmly to the damaged areas of corneal epithelium and basement membrane, forming corneal filaments. There may be grey sub-epithelial granular opacity, beneath the attachment to the corneal epithelium. Once established, corneal filaments are firmly attached to the underlying corneal epithelium. Friction between corneal filaments and the upper lid results in pain, epithelial tears and inflammation which leads to further filament formation.
Patients affected with filamentary keratitis are often highly symptomatic and may have persistent foreign body sensation, redness and sensitivity to light, which may vary from moderate to severe in intensity.
Filamentary keratitis can be a functionally debilitating and sight threatening feature of a number of ocular and systemic conditions such as:
- Keratoconjunctivitis sicca (dry eye syndrome): Both autoimmune (Sjögren syndrome) and non-autoimmune forms of aqueous-deficient dry eye conditions may have corneal filaments. This is the commonest cause of filamentary keratitis. Sjögren syndrome may be primary Sjögren syndrome when these changes occur in isolation, or secondary Sjögren syndrome when associated with connective tissue/ other diseases viz. systemic lupus erythematosus, polymyositis, juvenile chronic arthritis, Hashimoto’s thyroiditis or primary biliary cirrhosis.
- Superior limbic keratoconjunctivitis: Superior limbic keratoconjunctivitis is the second most common disease associated with corneal filaments.
- Exposure keratitis.
- Corneal oedema.
- Corneal surgery e.g. corneal refractive surgery.
- Post-cataract surgery.
- Use of contact lenses.
- Adenoviral keratitis.
- Herpes simplex keratitis.
- Bacterial keratitis.
- Neurotrophic keratopathy.
- Extended eyelid closure secondary to medications.
- Extended patching of eyes.
- Acne rosacea
- Systemic use of diuretics.
- Systemic use of antihistamines.
Filamentary Keratitis Symptoms |
- Foreign body sensation.
- Redness.
- Increased blinking.
- Discomfort.
- Lacrimation or watering.
- Photophobia (sensitivity to light).
- Blurring of vision.
- Blepharospasm (abnormal contraction of eyelid muscles).
Filamentary Keratitis Causes |
Filamentary keratitis is associated with a number of conditions or diseases associated with the ocular surface.
Aetiology of filamentary keratitis is related to:
- An alteration in the components of the tear film and /or
- Abnormalities of the corneal surface.
Common risk factors include:
- Aqueous tear deficiency: Aqueous tear deficiency as in keratoconjunctivitis sicca.
- Systemic diseases having effects on the corneal surface: Systemic diseases (e.g. Sjögren syndrome) having effects on the corneal surface.
- Corneal exposure: Corneal exposure as in seventh cranial nerve palsy.
- Ocular surgery: Ocular surgery (e.g. keratoplasty, cataract surgery).
- Anti-cholinergic medicines: Use of anti-cholinergic medicines for long periods.
- Ptosis (drooping) of upper eyelids: Ptosis (drooping) of upper eyelids may lead to poor tear distribution and reduction in oxygenation of the corneal epithelium.
The filaments are gelatinous and refractile in appearance and can vary from 0.5mm sessile adhesions to 10mm long strings. Filaments are generally attached to the basement membrane of the corneal epithelium at one end, with the other end freely moveable. Filamentary keratitis is associated with underlying basement membrane abnormalities, most of which are related to hypertonic tear film states. Filaments elongate and coil with movement of the eyelids.
The ratio of mucous to aqueous is usually increased because of:
- A decrease in aqueous tear production or
- Increased mucous production or
- Abnormal mucous accumulation.
A relative deficiency in the aqueous component of tear film is usually present in cases of filamentary keratitis, which produces a relative increase in the mucinous component.
Abnormalities of the ocular surface result in defects in the corneal epithelium that allow for anchoring of filaments.
Filamentary keratitis and dry eye:
Dry eye is the disorder most frequently associated with filamentary keratitis. There is increase in tear film osmolarity due to reduced aqueous tear secretion or increased tear film stasis, which leads to increase in mucous to aqueous ratio. This imbalance of mucous to tear ratio leads to sloughing of epithelial cells and produces epithelial defects. Mucous serves as a disposal system for exfoliated epithelial cells. Increase in viscosity of mucous enhances its adherence to irregularities on corneal epithelium, thus, potential for filament formation.
Filamentary Keratitis Diagnosis |
Diagnosis of filamentary keratitis is based on the clinical history and slit lamp examination (bio-microscopy), being conducted by an eye specialist.
Signs on slit lamp examination:
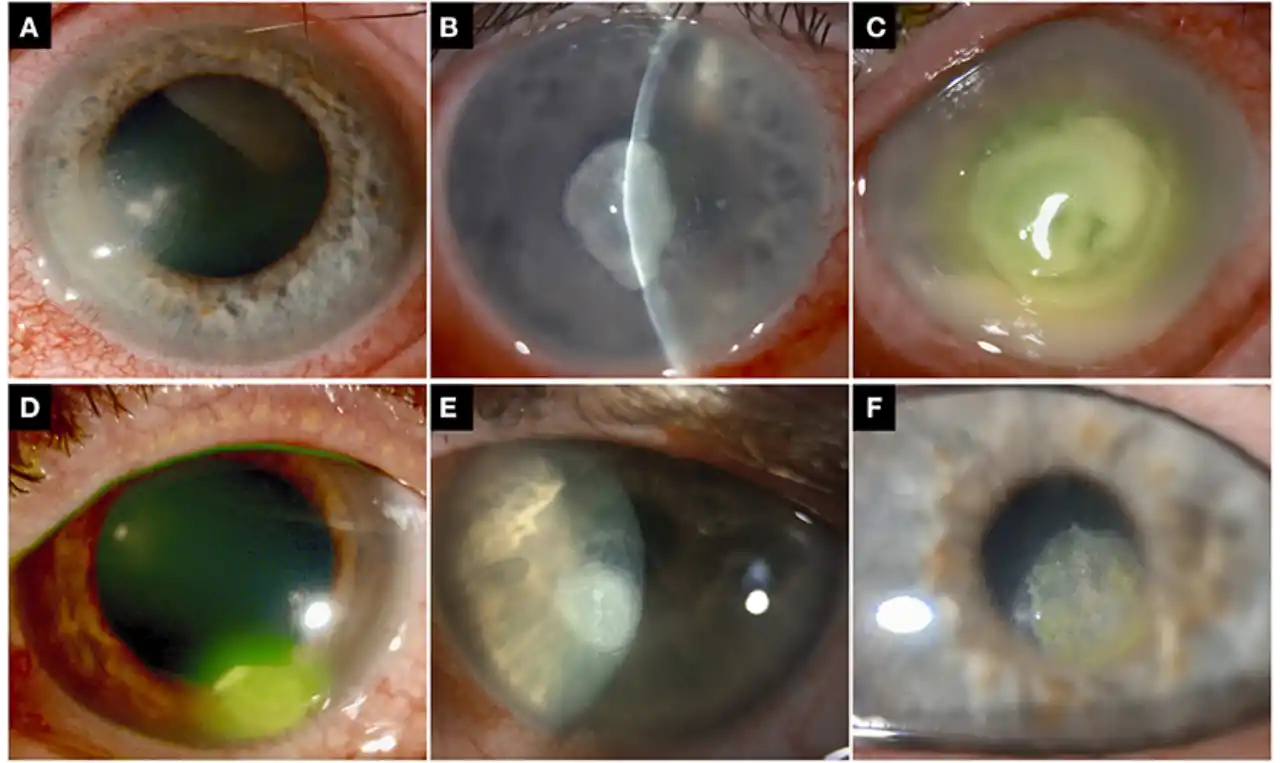
- Corneal filaments (mucoepithelioid strands): There may be multiple small, grey, mucoid filamentary attachments, firmly adherent to the corneal surface. Blinking causes painful traction on the filaments and may even detach them, leaving behind an epithelial corneal defect. Filaments may be stained best with rose bengal dye, but may be seen with fluorescein sodium and lissamine green stain as well.
Location of the filament may help determine the underlying cause,
Filaments in dry eye syndrome and exposure keratopathy: Filaments in dry eye syndrome and exposure keratopathy are usually found in the interpalpebral space.
Filaments due to ptosis, prolonged lid closure or superior limbic keratoconjunctivitis: Filaments due to ptosis, prolonged lid closure or superior limbic keratoconjunctivitis are seen superiorly on cornea.
Filaments due to ocular surgery: Filaments due to ocular surgery are found at the site of wound or surgical trauma.
For example, filaments following corneal transplantation are seen near sutures at the graft-host junction. After cataract surgery, they may be overlying or alongside the corneal incision. Surgery-specific factors, such as the disruption of proper tear flow, pooling, toxicity from medications, and local trauma, may predispose to filament formation.
- Decreased aqueous tears: There may be decrease in aqueous tears with abnormal tear break-up time (BUT).
- Increased mucinous element: Increased mucinous element in the pre-corneal tear film
- Superficial punctate keratopathy.
- Sub epithelial opacities: Sub epithelial opacities at the base of filaments.
- Epithelial defects: Frank corneal epithelial defects.
Histopathology:
Traditionally, it is said that the filament is composed of mucous and degenerated epithelial cells, and is adherent to the corneal epithelium at the base.
Wright used histochemical stains to suggest that filaments form when mucous in the tear film attaches to receptors on the corneal surface. Subsequent proliferation of a filament occurs as mucous accumulates cellular and other degenerative material. (Wright P. Filamentary keratitis. Trans Ophthalmol Soc UK 1975; 95: 260-266).
Zaidman et al. used electron microscopy to report that scattered groups of inflammatory cells and fibroblasts are present below the basement membrane of the corneal epithelium where filaments are attached (Zaidman GW, Geeraets R, Paylor RR, et al. The histopathology of filamentary keratitis. Arch Ophthalmol 1985; 103:1178-1181). It is suggested that an underlying pathological process damages the basement epithelium, leading to focal areas of its detachment from Bowman’s layer. This raised-epithelium subsequently becomes a nidus for mucous and degenerated cells.
Tanioka et al. proposed that corneal epithelium cells form the core of the filament and an admixture of multiple surface mucins, deoxyribonucleic acid (DNA) material, and degenerated conjunctival epithelial cells become wound around the core to produce a braided shape (Tanioka H, Yokoi N, Komuro A, et al. Investigationof the corneal filament in filamentary keratitis. Invest Ophthalmol
