What is Amaurosis Fugax ?
Amaurosis Fugax or transient monocular blindness (TMB) refers to transient brief blindness, blurring, fogging, or dimming of vision, varying in duration from few seconds to minutes or even hours in some cases. The duration of visual impairment is brief usually less than fifteen minutes and rarely exceeding thirty minutes. The term Amaurosis fugax has been used not only for monocular condition, but also for the transient loss of vision in both eyes (less common). Most of the patients are affected for about one to five minutes only. Generally, recovery is in the same pattern as the visual loss, although usually more gradual. Amaurosis is also known as blackout.
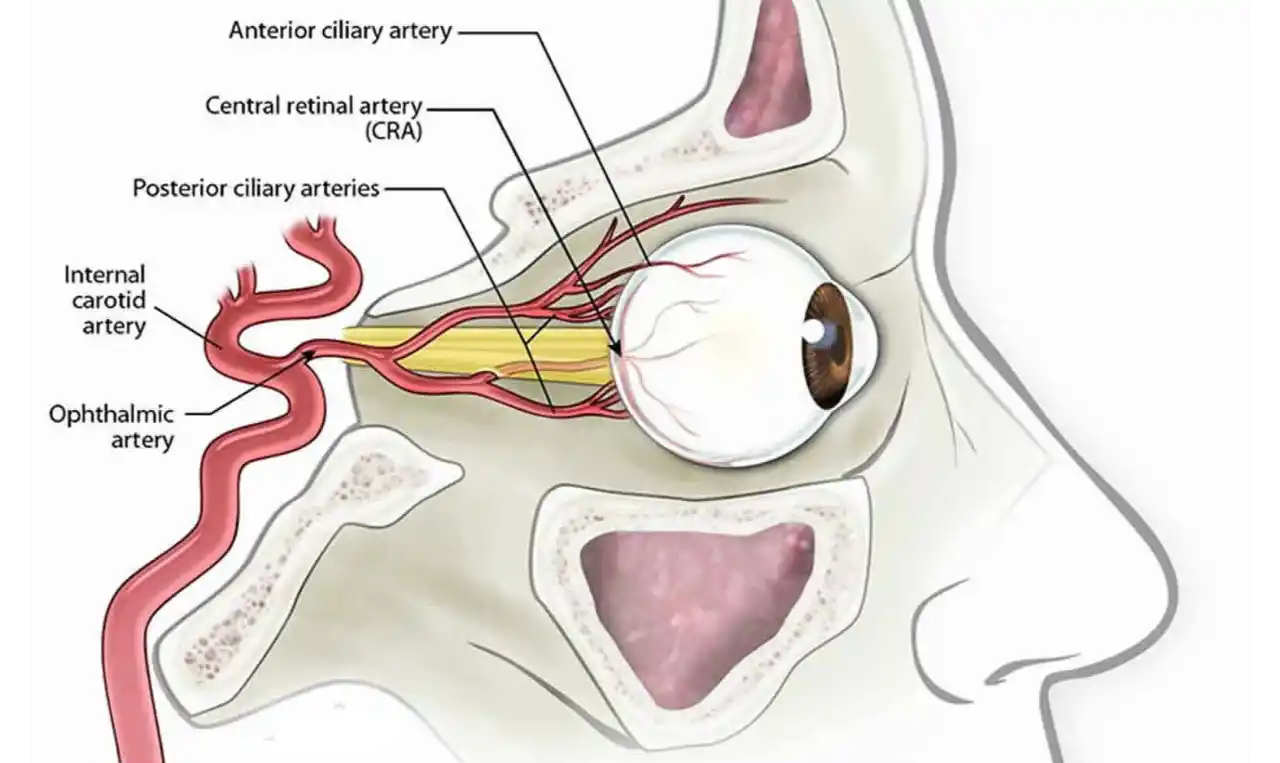
It is thought to occur from transient occlusion of the ophthalmic circulation and is a risk factor for acute stroke. Fundus examination is commonly normal but may show prior retinal arterial emboli or attenuation of arteries. Investigations like carotid ultrasonography and cardiac echography may help in finding source of embolus.
It is produced by ocular vascular occlusive disorders such as
- Central retinal artery (CRA) occlusion
- Central retinal vein (CRV) occlusion
- CRV occlusion with cilioretinal artery occlusion
- Branch retinal arteriole occlusion
- Branch retinal vein occlusion
- Ocular ischaemic syndrome (OIS)
- Arteritic and non-arteritic anterior ischaemic optic neuropathy (AION)
It may also be seen in giant cell arteritis.
Detailed history of Amaurosis attack and the duration of visual disturbance helps in classification of visual loss occurrence into following four types
Type I: It is due to transient retinal ischaemia
Type II: It is due to retinal vascular insufficiency
Type III: It occurs due to vasospasm
Type IV: It occurs in association with antiphospholipid antibodies but also include cases due to unknown causes.
Amaurosis Fugax Symptoms
Symptoms vary according to the type of Amaurosis depending upon visual loss occurrence:
Type I: It is characterised by sudden brief attack of partial or complete diminution or obscuration of vision, lasting for seconds to minutes, followed by total recovery. Partial impairment presents as ascending or descending curtain or a blind moving sideways across the eye. Visual field defect is complete or partial. It is due to retinal ischaemia, embolisation or arteritis.
Type II: It is less rapid in onset and may be associated with loss of contrast vision and photopsiae. It lasts from minutes to hours. Pain may be rarely associated and the recovery is complete. Visual field defect is complete or partial. It is produced due to retinal hypoperfusion and carotid occlusive disease.
Type III: It is of abrupt onset and show photopsiae, scintillating sparkles, and is often accompanied by pain. It is due to vasospasm and migraine. Visual field defect is complete and may lead to progressive contraction. It lasts for minutes only and the recovery is usually complete.
Type IV: It is of abrupt onset and may alternate between two eyes. It occurs in association with antiphospholipid antibodies but also include cases due to unknown causes. Visual field defect may resemble any of the types from one to three as mentioned above. Duration may go up to any length of time and the recovery is complete.
Amaurosis Fugax Causes
The causes of Amaurosis fugax are divided into five groups
- Embolic
- Haemodynamic
- Neurologic
- Ocular
- Idiopathic
Usually Amaurosis fugax is typically used to refer to transient visual loss of embolic origin. Episodic attacks of blindness occur as arteriosclerotic plaques progressively narrow the lumen of ipsilateral internal carotid artery (ICA), leading to reduced pressure and flow in ophthalmic artery. Cholesterol crystals (Hollenhorst plaques) or ulcerating plaque may embolise to ophthalmic or central retinal artery, without causing permanent visual loss.
TMB is regarded as one variety of transient ischaemic attack (TIA) and should be recognised as a warning sign of impending stroke. Frequency of attacks may vary from several times in a day to once only every few months. Cerebral ischaemia may affect both eyes with ipsilateral hemifield defect.
Amaurosis usually occurs in elderly patients over fifty years of age who have vascular risk factors such as hypertension, hypercholesterolaemia, history of smoking, or previous episodes of TIAs.
Amaurosis Fugax Diagnosis
Diagnosis depends upon clinical history and examination.
Patients present with sudden monocular loss of vision that usually is less than fifteen minutes, and it rarely exceeds thirty minutes. Vision loss may be complete or partial. It is described as a curtain falling down in front of the eye or as a generalised darkening. Patient may experience one to multiple episodes, which usually resolve spontaneously. The attacks may sometimes be associated with ipsilateral cerebral TIA, with contralateral neurological features.
Some patients may present with emboli such as cholesterol plaques, which may result in retinal ischaemia. Depending upon the severity of ischaemia, BRA or CRA occlusion may develop.
Other group of patients, mainly with ocular ischaemic syndrome, ipsilateral internal carotid artery occlusion produces hypoperfusion to retinal photoreceptors with resultant blurring or diminution of vision. Patients with ocular ischaemic syndrome present with transient blurring of vision. Vision deteriorates with progression of disease. Episcleral vessels may show congestion and there may be mild anterior chamber inflammation. Fundus examination usually shows dilated and tortuous retinal veins with narrowed arterioles and dot/blot haemorrhages. Persistent hypoperfusion may lead to development of neovascularisation in iris, angle of anterior chamber, optic disc, and retina.
The visual loss from migraine may last from few seconds to an hour. It is preceded by a scintillating scotoma, or is precipitated by exercise or rise in body temperature (Uhthoff sign).
Patients with giant cell arteritis may show palpable hard arteries or tenderness of scalp.
Investigations
Besides general examination, following investigations may help in assessment of vessels.
- Doppler test: Doppler of carotid vessels may help in assessment of vessels.
- Magnetic resonance imaging: It may help in assessment of vascular patency.
- Computed tomography: Vascular patency may also be assessed by computed tomography.
- Electrocardiogram/ Holter monitoring: This helps to localise any cardiac arrhythmia or any possible source of cardiac emboli.
- Neuroimaging: It may be done to rule out any other cause of vision loss.
Differential diagnosis
Besides CRA/CRV occlusion, monocular vision loss may be due to conditions such as
- Papilloedema
- Multiple sclerosis
- Sickle cell anaemia
- Epilepsy
